Hip Pain is one of the main reasons patients come to our practice for help. Identifying the cause of your hip pain is important because different causes of hip pain are treated differently. Whilst there are many potential causes of hip pain, our experience helping patients with hip pain for over 12 years tells us that three problems account for the vast majority of patients coming to us for help with their painful hip. In this article we discuss the three most common causes of hip pain we see in our practice as well how physiotherapy can help for each.
1. The Lower Back
Why are we discussing the lower back in an article about hip pain? There are two main reasons: Firstly, where you feel pain in your body is not necessarily where the problem is. The concept of referred pain applies to the hip, where you may feel pain somewhere in your hip but the problem is actually referred from your lower back. Second, what many patients describe as their hip is not actually their hip at all, but often the base of their spine or lower back. This is especially true if your pain is on one side of your body and you feel it near the dimple in your lower back or somewhere in your buttock. For more information on how we treat lower back pain, read our article by clicking here.
How do I know if my lower back is causing my hip pain?
Because of the reasons outlined above, one of the things we must do for every hip pain patient is screen their lower back to see if it could be the source of their pain. This process involves asking specific questions about the location of your pain, which activities and positions make you feel worse, your past history and how this current problem came about. After taking a thorough history we guide you through a lower back movement screen plus some special tests. If we reproduce your usual “hip” pain by moving or testing your lower back, it means that your lower back is relevant to your hip problem and treatment should begin with the lower back rather than the hip. Sometimes patients may have two sources of pain – their lower back AND their hip. For these patients we need to decide which of these two areas is most important and treat that area first.
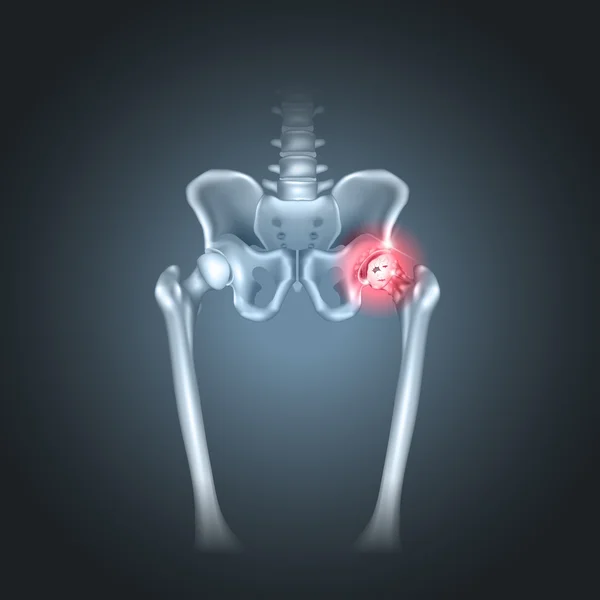
2. Hip Osteoarthritis
Osteoarthritis (OA) is a condition that affects the major joints of the body and is characterised by loss of the hard wearing cartilage that lines the ends of the bones forming a joint. OA is not just about cartilage loss, however — changes occur in the supporting tissues of the joint, including the capsule and ligaments, as well as the supporting muscles. Any of these structures can be a source of pain in hip OA.
How do I know if I have Hip Osteoarthritis?
The diagnosis of hip OA is made on several features, but first we have to rule out the lower back as a source of your pain. Once we have done this, we can start to think about what type of hip problem you have. Hip OA is characterised by activity-related pain in or around the hip (often in the front of the hip) in patients over 50 years of age. You may have pain walking, getting in or out of your car, going up or down stairs or dressing yourself. An x-ray should show the hallmark features of osteoarthritis. Other causes of hip pain need to be excluded — this is done by taking a careful history and, if needed, ordering other tests. In your physical examination you should have loss of movement in your hip joint with pain and/or stiffness, usually in a particular pattern.
Can Physio help if I have Hip Osteoarthritis?
Although we have no cure for osteoarthritis, physiotherapy can help patients improve their function and reduce their symptoms. The main goals in physiotherapy are to restore the best possible movement in your hip, strengthen the supporting muscles around your hip and correct any faulty movements, like your walking pattern or how you negotiate stairs. Treatment usually involves targeted stretching and movement of the affected hip, a home exercise program that includes both strengthening and stretching, and advice on your activities. We typically see patients weekly or fortnightly for several months in an effort to get you moving and feeling as best as possible. For more information on hip osteoarthritis read our article on this particular topic by clicking here.
3. Gluteal Tendinopathy
Gluteal Tendinopathy is a condition affecting one or two of the gluteal tendons — the strong bands of tissue that connect your hip muscles to the bony outside point of your hip. In some patients these tendons are sore and swollen, whereas in other patients there may be a small tear in the tendon. Patients with gluteal tendinopathy describe pain on the outside of the hip, in the buttock and often down the outside of the leg. Gluteal tendinopathy affects women in their forties and fifties – men do develop this problem but often a little bit later in life (in their 60’s and 70’s).
How do I Know If I have Gluteal Tendinopathy?
Gluteal tendinopathy is a common condition and a diagnosis can be made without an x-ray or ultrasound. Often there is no specific injury but the patient will describe their hip becoming worse with activity and also at night. There are several physical tests for gluteal tendinopathy and if you test positive for two or more of these our confidence about your diagnosis is high. Your doctor may order an ultrasound of your hip but beware – it is normal to see some age-related changes in the gluteal tendon even when it isn’t sore, so you should never rely on your ultrasound alone to make a diagnosis. As mentioned above, in making a diagnosis of gluteal tendinopathy we also have to rule out other areas – like your lower back and hip joint.
Can Physio help if I have Gluteal Tendinopathy?
Most patients with gluteal tendinopathy get better with the help and guidance of a good physio. Treatment should follow three stages:
- Decrease pain and Inflammation
- Restore strength, and
- Return to Normal activities.
There are key things to do in each stage and you need to be patient! A common mistake patients make is they complete stage 1 (meaning they no longer have pain at night and can do their everyday activities) but then skip stage 2 and try and return to their normal activities as soon as their pain settles. If you DON’T restore strength in your hip before returning to normal activities the pain often comes back! For more information on gluteal tendinopathy read our article on this particular topic by clicking here.
What to do next:
Understanding the physical cause of your hip pain is important and we know from treating patients for over 12 years that patients want a clear diagnosis of explanation for their pain. From a physiotherapy perspective, a clear diagnosis is the first step to solving your pain, because it informs or directs your treatment. Getting the right treatment for the wrong problem is a common mistake in physiotherapy – we avoid this by taking extra time in our initial appointment to take a very thorough history, complete a targeted physical examination and look at any imaging you have already had.
If you are experiencing trouble with hip pain, reach out and call us today on 6056 6616. Our helpful front desk team will help you find a day and time that works for you to come in and see one of our experienced physio’s and get you started on moving and feeling better! If you would like to see our physio’s in action, watch one or more of our videos on how to do common hip exercises by clicking here.
To Your Better Health,
The Team at Personal Best Physiotherapy