Physio Referrer Online-
Reducible Discogenic Pain: What is it, how to recognise it and what to tell your patients
Low back pain (LBP) remains the most common presenting problem to our practice. The reliable identification of subgroups of patients with LBP who are likely to respond to targeted treatment remains a priority of primary care. In this issue of Physio Referrer, we review the clinical diagnosis of Reducible Discogenic Pain (RDP). If you are aware of the key features of this diagnosis you can direct your patients to physiotherapy as well as advise them on ways the can help themselves.
What is Reducible Discogenic Pain?
Described by Ford, Surkitt and Hahne (2011), RDP describes a group of patients with low back pain who respond to specific mechanical loading strategies – movements and positions that have a positive effect on their symptoms, movements and function. This is a clinical diagnosis, not a radiological one, and is based on an understanding of the lumbar intervertebral disc including normal mechanics as well as pathology.
Do you recognise this patient?
Patients with RDP present with low back pain but no symptoms of radiculopathy (no neurological symptoms and no symptoms below the level of the knee). This is an important distinction, as the presence of radiculopathy will influence the treatment pathway of your patient. The most typical location of symptoms would be the lower back, often radiating outwards along the pelvic crest and sometimes into the buttock. Their symptoms maybe more intense on one side and sometimes shift from one side to the other.
Key features of the patient’s history include repetitive flexion (working in the garden on the weekend), sustained sitting (a long car drive or international flight) or doing an activity they are not accustomed to. These patients don’t like sitting for very long and their back often feels stiff and sore in the morning. They have difficulty with most flexion activities, from putting on their shoes and socks on to gardening and lifting. Variability in symptoms behaviour is a key feature of discogenic pain and this is important to acknowledge, as patients are sometimes confused as to why their back feels good one day, then stiff and sore the next.
How do we treat these patients?
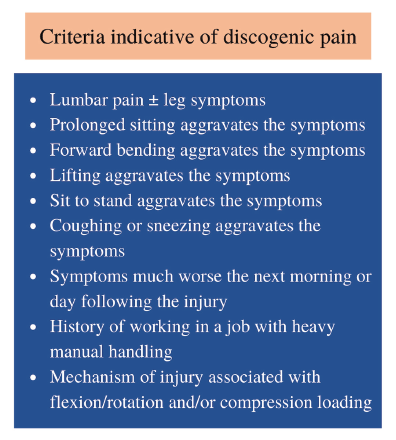
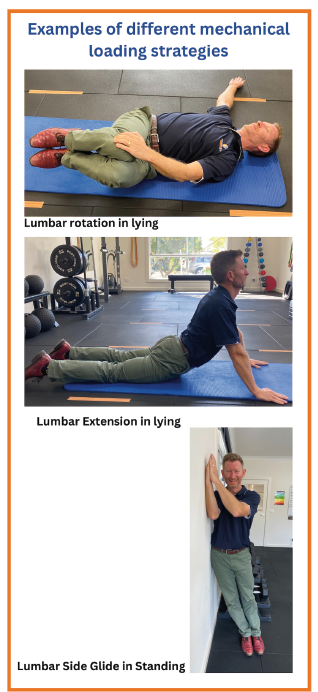
As mentioned above, these patients demonstrate a positive response to specific mechanical loading strategies. The most common loading strategy required to help these patients is some form of lumbar extension, but this is not ALWAYS the case- some patients need a LATERAL strategy and others need ROTATION (see photos). The key is finding the mechanical strategy that reduces your patients symptoms and improves their mechanics, Improvement can occur within one session or sometimes over a week or two applying the recommended loading strategy.
Patients are instructed to complete their specific exercise or positioning at home regularly (3-5 times a day), with reassessment usually occuring within a week. If they initially respond to targeted exercise but then plateau, progression of the loading strategy is indicated. This may be a progression of force, or in some instances addition of a second component to get the best clinical effect. The goal is to restore full pain free movement of the lumbar spine over several sessions.
What can you tell your patients?
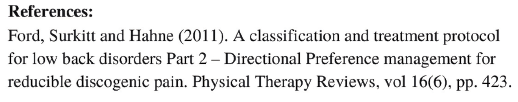
If your patient with low back pain has 4 or more of the criteria for discogenic pain listed in the table above, and you have rulled out serious or sinister pathology, you can confidently refer them to physiotherapy. In addition, you can also advise them to reduce their total daily sitting by 50%, encourage them to do a gentle activity like walking , and of course use simple analgesia such as paracetamol and/or NSAID. You can also ask them to look out for their symptoms centralising -(moving to the centre of the lower back) and remind them that this is a very good sign of recovery, even if their pain feels temporarily a little worse in their lower back area.
If you have a particular patient with LBP who you are unsure about, please call us on 6056 6616- after a brief chat over the phone we can usually advise you if your patient should attend physiotherapy or not.